Chapter 6: PALS-Airway Management
In Pediatric Advanced Life Support (PALS), airway management is crucial for maintaining or establishing a clear airway in patients who are unconscious or unable to maintain airway patency on their own. This involves a range of approaches, from noninvasive techniques to more invasive measures, often performed simultaneously or in rapid succession. The choice of intervention depends on the patient’s condition, the expertise of the healthcare provider, and the availability of resources. Effective airway management is essential for ensuring adequate oxygenation and ventilation.
Techniques of Opening the Airway:
| Aspect | Jaw Thrust | Head Tilt-Chin Lift |
|---|---|---|
| Purpose | Open the airway without movement of the cervical spine | Open the airway by tilting the head backward and lifting the chin upward |
| Indications | Suspected cervical spine injury or trauma | No suspected cervical spine injury |
| Patient Position | Supine position | Supine position |
| Technique |
1. Place fingers behind the angle of the jaw on both sides. 2. Lift the jaw forward, keeping the mouth closed. 3. Avoid movement of the head and neck. |
1. Place one hand on the patient's forehead, and the other hand under the bony part of the chin. 2. Tilt the head backward while lifting the chin upward. 3. Ensure a sniffing position by tilting the head back. 4. Keep the mouth open for ventilation. |
| Contraindications | None | Suspected cervical spine injury or trauma |
| Complications/Risks | Limited risk of exacerbating cervical spine injury if not done correctly | Limited risk of exacerbating cervical spine injury if not done correctly |
| Notes | Preferred in situations where cervical spine injury is suspected | Commonly used in basic life support situations where cervical spine injury is not suspected |
Methods of Oxygen Delivery
OXYGEN IS THE #1 DRUG – GIVE OXYGEN AS SOON AS IT IS AVAILABLE!
| Device | Low-flow Nasal Cannula
|
High-flow Nasal Cannula
|
Simple Oxygen Face Mask
|
Non-Rebreather Mask
|
BVM Resuscitator
|
|---|---|---|---|---|---|
| Description | Two small prongs inserted | Two small prongs inserted | Dome-shaped mask over | Face mask with reservoir bag | Handheld device with mask and reservoir bag |
| Flow Rate (L/min) | 1–4 | 2–8 | 6–10 | 10–15 | ≥ 15 |
| Oxygen Concentration (%) | 22–44 | >45 | 35–55 | Up to 90 | ≥ 90 |
| Suitability | Mild to moderate hypoxia | Moderate to severe hypoxia | Moderate to severe hypoxia | Moderate to severe hypoxia | Severe hypoxia |
| Use Case | Low-flow | High-flow | Low-flow | High-flow | High-flow |
| Special Features | Lightweight, flexible tubing | Heated and humidified air for improved comfort | Simple design, easy to use | One-way valves prevent exhaled air from entering bag | Allows manual ventilation of the patient |
| Advantages | Well-tolerated for extended use | Precise and higher oxygen delivery in critical care settings | Easy application, good for short-term use | High concentration of oxygen delivered | Provides positive pressure ventilation |
| Disadvantages | Limited oxygen concentration | May be less comfortable for extended use | May cause discomfort, not suitable for patients with CO2 retention | Risk of suffocation if reservoir bag is deflated | Requires training for proper use |
| Notes | Commonly used for respiratory conditions requiring low oxygen support | Utilized in critical care settings, post-surgery, or during procedures requiring high oxygen flow rates | Suitable for stable patients requiring moderate oxygen | Used for high-concentration oxygen delivery | Essential in Pediatric advanced life support scenarios |
Airway Adjunct:
During Pediatric Advanced Life Support (PALS), effective airway management is integral to the overall resuscitation efforts. The terms OPA (Oropharyngeal Airway) and NPA (Nasopharyngeal Airway) refer to airway adjuncts used to maintain or establish a patent airway. These devices play a crucial role in managing the airway during respiratory emergencies or cardiac arrest. An OPA is inserted into the mouth and is used in unconscious children without a gag reflex to keep the tongue from obstructing the airway. An NPA, inserted through the nostril, is useful in conscious, semi-conscious, or unconscious children as it can maintain an open airway without triggering a gag reflex. Proper use of these airway adjuncts helps ensure adequate ventilation and oxygenation, which are essential components of effective resuscitation in PALS.

Nasopharyngeal Airway-
| Aspect | Nasopharyngeal Airway (NPA) in PALS |
|---|---|
| Purpose | Maintain airway patency for unconscious, conscious, or semi unconscious patients |
| Indications | Unconscious, conscious, or semi unconscious patients requiring airway support |
| Insertion Technique | 1. Measure from the corner of the nose to the tragus of the ear |
| 2. Choose size based upon the diameter of the nostril (a 12F or 3mm will generally fit a full term infant) | |
| 3. Gently insert through one nostril, directing posteriorly | |
| 4. Secure in place and monitor for discomfort or complications | |
| A shortened E.T. tube may be used | |
| Removal | Remove upon regaining consciousness and ability to maintain a clear airway independently |
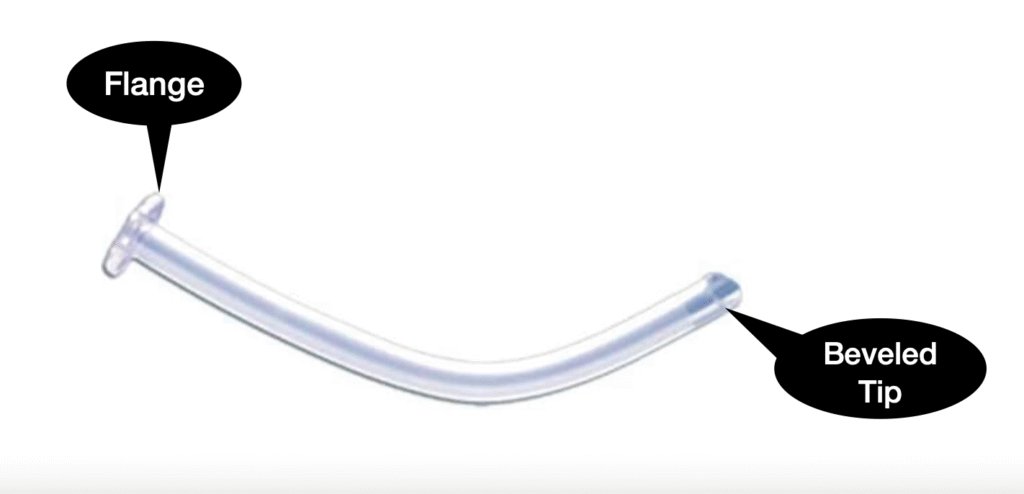
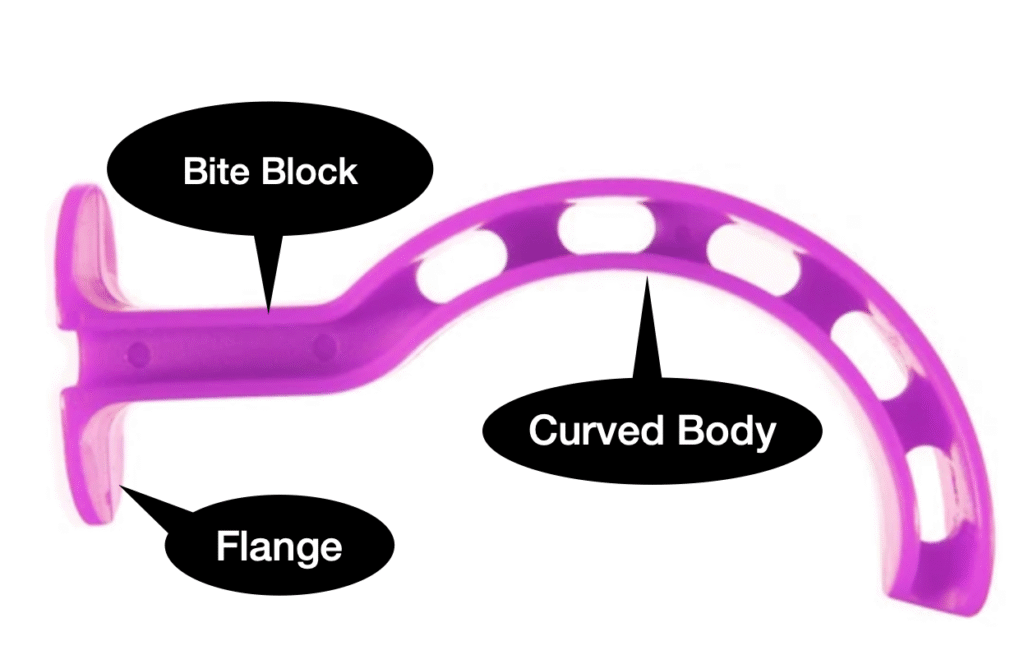
Oral pharyngeal Airway-
| Aspect | Oral Pharyngeal Airway (OPA) in PALS |
|---|---|
| Purpose | Maintain airway patency for unconscious patients |
| Indications | Unconscious patients requiring airway support |
| Insertion Technique |
1. Measure from the corner of the mouth to the angle of the jaw 2. Choose the appropriate size 3. Insert while using a tongue depressor to hold the tongue on the floor of the mouth 4. Insert the OPA with the curve facing the hard palate 5. Rotate 180 degrees to follow the natural curvature of the mouth 6. Ensure flange rests against the lips to prevent deep insertion 7. Secure in place and monitor for discomfort or complications |
| Contraindications | Presence of a strong gag reflex |
| Complications | Gagging or vomiting during insertion |
| Notes |
Regular assessment and monitoring are essential It is still necessary to keep the head and neck in the sniffing position after the oral pharyngeal airway is in place Do not suction for more than 10 seconds at a time Reposition or remove if the patient regains consciousness or complications arise |
| Removal | Remove if the patient regains consciousness and can maintain a clear airway independently |
PALS Airway Intubation:

Airway management is a critical aspect of pediatric emergency medical care, and several devices are available for securing the airway in patients requiring intervention. Among these devices are the laryngeal mask airway (LMA), laryngeal tube (LT), esophageal-tracheal combitube (ETC), and endotracheal tube (ETT).
Estimating Endotracheal Tube Size in Children
For children aged 2 to 10 years, the appropriate internal diameter (ID) of the endotracheal tube (ETT) can be estimated using the following formulas:
- Uncuffed ETT size (mm ID):
(Age in years÷4)+4 - Cuffed ETT size (mm ID):
(Age in years÷4)+3.5
Remember: Cuffed tubes should not be inflated to a pressure >20 cm H2O.
These airway devices are integral to ensuring effective ventilation and oxygenation during pediatric emergencies, each offering unique benefits and applications based on the specific clinical scenario.
Notes:
● Intubation attempts should be limited to 30 seconds.
● If bradycardia develops or the clinical condition of the child being intubated deteriorates, interrupt the intubation attempt to provide bag-mask ventilation with 100% oxygen.
● Insertion of an advanced airway may be deferred until several minutes into the attempted resuscitation, since airway Insertion requires an interruption in chest compression for longer than 10 seconds.
● Auscultation of lungs for bilateral breath sounds.
● Auscultation of the gastric area – no gurgling should be heard that would indicate intubation of the esophageal area.
DOPE:
If deterioration in respiratory status occurs in an intubated child, use the DOPE mnemonic:
- D – Displacement: Ensure proper placement, especially in uncuffed ETT tubes which can easily become displaced.
- O – Obstruction: ETTs in children can become occluded.
- P – Pneumothorax: If breath sounds are diminished on one side, consider needle decompression.
- E – Equipment: Ensure all equipment is functioning properly.
| Feature | Laryngeal Mask Airway (LMA) | Laryngeal Tube (LT) | Esophageal-Tracheal Combitube (ETC) | Endotracheal Tube (ETT) |
|---|---|---|---|---|
| Insertion Difficulty | Easy | Easy | Moderate | Difficult |
| Placement Verification | No direct visualization of trachea | No direct visualization of trachea | No direct visualization of trachea | Direct visualization of trachea |
| Cuff Inflation | Inflatable cuff at distal end | Inflatable cuff at distal end | Double-lumen design with distal cuff | Inflatable cuff at distal end |
| Anatomical Seal | Seals around laryngeal inlet | Seals around laryngeal inlet | Seals in esophagus and trachea simultaneously | Seals within trachea |
| Contraindications |
- Known or potential difficult airway - Full stomach or increased risk of aspiration - Risk of regurgitation/vomiting - Limited mouth opening or obstruction - Unconscious or unresponsive patient - Need for positive pressure ventilation - Need for prolonged airway management |
- Known or potential difficult airway - Full stomach or increased risk of aspiration - Risk of regurgitation/vomiting - Limited mouth opening or obstruction - Unconscious or unresponsive patient - Need for positive pressure ventilation - Need for prolonged airway management |
- Known or potential difficult airway - Full stomach or increased risk of aspiration - Risk of regurgitation/vomiting - Limited mouth opening or obstruction - Unconscious or unresponsive patient - Need for positive pressure ventilation - Need for prolonged airway management |
- Facial trauma or deformity - Basilar skull fracture - Cervical spine injury - Unstable neck - Glottic or subglottic pathology - Suspected or confirmed cervical spine injury - Trismus (difficulty opening mouth) - Burn or smoke inhalation injury |
| Who Can Perform | - Generally, trained healthcare providers, including physicians, nurses, paramedics, and respiratory therapists | - Generally, trained healthcare providers, including physicians, nurses, paramedics, and respiratory therapists | - Generally, trained healthcare providers, including physicians, nurses, paramedics, and respiratory therapists | - Typically, advanced healthcare providers with specific training, including physicians, anesthesiologists, and advanced practice nurses |

PALS Suctioning Techniques:

In the context of PALS, suctioning plays a crucial role in airway management, particularly during cardiac arrest and other emergency situations.
Here’s an overview of suctioning in PALS:
Purpose of Suctioning in PALS:
1. Clearing Airway Obstruction:
– Suctioning is employed to remove secretions, blood, vomitus, or other foreign materials that may obstruct the patient’s airway.
– Airway patency is essential for effective ventilation and oxygenation during resuscitation efforts.
2. Facilitating Ventilation:
– In scenarios where a patient’s airway is compromised by fluids or debris, suctioning helps ensure unobstructed airflow for ventilation.
– Effective ventilation is critical in maintaining oxygenation and preventing hypoxia.
3. Enhancing Visualization:
– During advanced airway procedures such as endotracheal intubation, suctioning assists in clearing the airway for better visualization of the vocal cords and tube placement.
Procedure for Suctioning in PALS:
Assessment:
– Evaluate the need for suctioning based on clinical signs such as gurgling sounds, visible secretions, or airway obstruction.
Prepare Equipment:
– Ensure the suction unit is functional and properly connected.
– Choose an appropriate suction catheter size for the patient.
Position the Patient:
– Position the patient appropriately to facilitate suctioning, considering the patient’s condition and any ongoing resuscitation efforts.
Preoxygenation:
– Administer high-flow oxygen to the patient before and after suctioning to optimize oxygen levels.
Suctioning Technique:
Suctioning is carried out utilizing either a flexible or rigid catheter connected to a suction unit, which can be wall-mounted or portable. The suction unit is equipped with a pressure gauge to indicate the negative pressure (suction force) and a collection canister.
– Flexible Catheters:
– Suitable for eliminating thin, fluid secretions from the oropharynx or nasopharynx.
– Inserted through the mouth or nose.
– A sterile flexible catheter is employed for suctioning an endotracheal tube.
– Rigid (Yankauer) Catheters:
– Designed for removing thick or particulate matter from the oropharynx.
– Inserted through the mouth.
– Insert the suction catheter into the airway while applying intermittent suction during withdrawal.
– Limit each suctioning pass to 10 seconds to minimize the risk of hypoxia.
– Monitor the patient’s oxygen saturation and vital signs throughout the procedure.
Repeat as Needed:
– Repeat suctioning as necessary, reassessing the airway and patient response.
Post-Suctioning Care:
– Provide additional oxygen and reassess the effectiveness of ventilation.
– Address any ongoing airway management needs.
Considerations:
– Suctioning should be performed cautiously to prevent complications such as hypoxia or tissue trauma.
– Regular reassessment of the airway and the patient’s response is essential during suctioning in PALS.
Suctioning is a vital component of airway management in PALS, ensuring the maintenance of a clear and patent airway during resuscitation efforts. It is crucial for healthcare providers to be proficient in suctioning techniques and integrate them seamlessly into the overall care of the patient in emergency situations.
Waveform Capnography:
What is Waveform Capnography?
Waveform capnography measures the amount of carbon dioxide (CO2) in exhaled air, which provides information about the patient’s ventilatory status. It displays this information in both numerical form (end-tidal CO2, or EtCO2) and as a waveform, allowing for continuous monitoring.
Components of the Capnography Waveform
The capnography waveform, also known as a capnogram, consists of several phases:
1. Phase I : Baseline, representing exhalation of CO2-free gas from the anatomical dead space.
2. Phase II: Expiratory upstroke, where CO2 from alveolar gas starts to mix with dead space gas.
3. Phase III: Alveolar plateau, where alveolar gas is exhaled and the CO2 level reaches a plateau.
4. Phase IV: Inspiratory downstroke, where fresh gas without CO2 is inhaled.
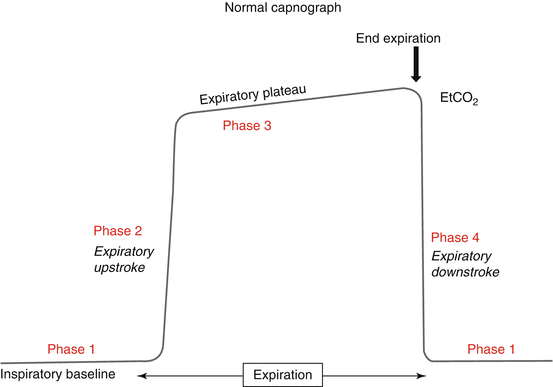
Clinical Uses in PALS
1. Verification of Endotracheal Tube Placement:
● A consistent waveform and an EtCO2 value between 35-45 mmHg indicate correct tube placement.
● Absence of a waveform or a sudden drop in EtCO2 can indicate dislodgement or obstruction of the tube.
2. Monitoring Quality of CPR:
● During cardiac arrest, capnography helps monitor the effectiveness of chest compressions.
● Higher EtCO2 values (e.g., >10 mmHg) indicate effective chest compressions and adequate blood flow.
● Sudden increases in EtCO2 during resuscitation can suggest a return of spontaneous circulation (ROSC).
3. Assessing Ventilation:
● Capnography provides real-time feedback on ventilation status, helping adjust ventilation rates and tidal volumes.
● It can help identify hypoventilation (elevated EtCO2) or hyperventilation (decreased EtCO2).
● Always monitor a patient with pulse oximetry When possible, monitor with capnography.
4. Detecting Respiratory Conditions:
● Changes in the capnogram shape can indicate airway obstruction, bronchospasm (e.g., asthma), or other respiratory conditions.
Interpretation in PALS Scenarios
● Normal Values: EtCO2 of 35-45 mmHg and a rectangular waveform.
● Hyperventilation: EtCO2 < 35 mmHg, shorter waveform.
● Hypoventilation: EtCO2 > 45 mmHg, taller waveform.
● Flat Line: Indicates no CO2 detected, possible dislodged tube or no circulation.
Incorporating waveform capnography into PALS protocols enhances patient safety and improves outcomes by providing real-time, continuous feedback on ventilation and circulation status.